By Will Flanders and Rick Esenberg
In the modern information environment, it is challenging to find any source of objective information. On no issue is this more true than with the COVID-19 pandemic. On one side are those wedded to “the science” until it disagrees with their preconceived notions about what policy ought to be. On the other side are those who, rightfully skeptical of government, reject most all information that makes the case that COVID-19 is still a major problem. We are a polarized country and the most engaged people tend not to want to hear – or reward – nuance. But there are times when a rigorous examination of the facts compels a nuanced conclusion. Let’s take a look at the most recent COVID numbers in Wisconsin.
1. Vaccines DO provide protection
Some have noted that the data shows coronavirus rates are increasing most rapidly among the vaccinated. This is true, but what does it mean? It is still the unvaccinated that are driving the continuance of the pandemic. Recently, the Department of Health Services put out a chart that shows the rate of cases, hospitalizations, and deaths among the vaccinated and unvaccinated cohorts in the state. That chart is reproduced below.
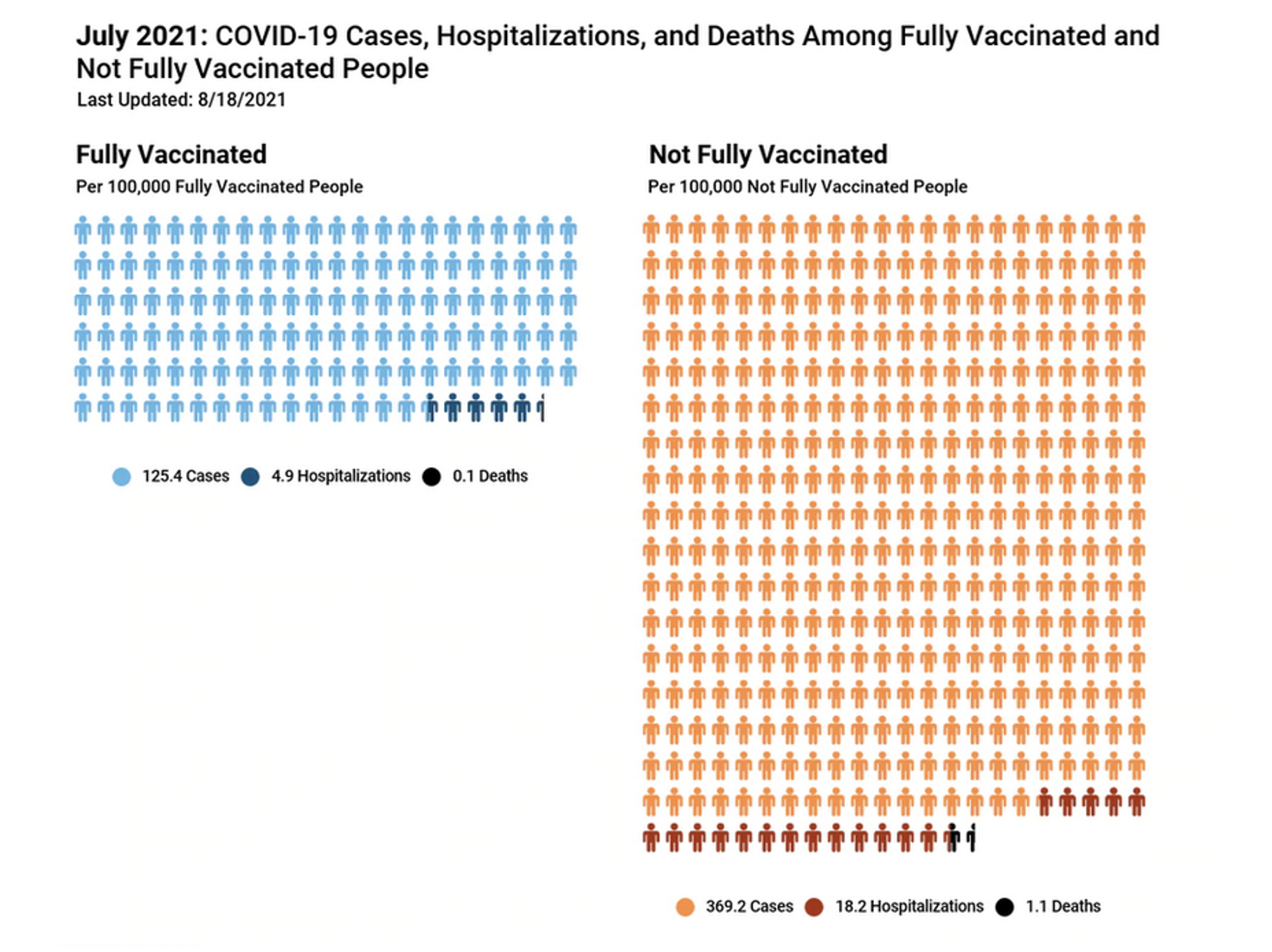
Among the fully vaccinated, the number of cases per 100,000 was roughly one third of the total for those that are not fully vaccinated. The rate of hospitalizations was 378% lower. The rate of deaths was 1100% lower. Indeed, the notion that the death rate for vaccinated persons is “effectively zero” is supported by the Wisconsin data. The vaccines work.
Why then, are rates increasing faster among the vaccinated? The answer is that the vaccinated group is starting from a very low rate of infection. According to DHS, the number of cases per 100,000 has gone from 14.4 in June to 125.4 among the vaccinated, while going from 82.8 in June to 369.2 among the non-vaccinated. The rate has assuredly increased faster among the vaccinated, but cases among the non-vaccinated grew by about 280 per 100,000 compared to 121 per 100,000 among the vaccinated. Public health researchers have long cautioned against using percentage changes in this way to evaluate the effectiveness of a healthcare intervention, and to do so is misleading.
2. The Virus is Becoming Less Deadly
Despite the doom-and-gloom of the preceding paragraphs, the good news is that the rate of deaths from the virus continues to decline. In Florida, the state cited most often in the news media as the current center of the pandemic, the rate of deaths has actually declined substantially in the past week even as case counts continue to grow. The figure below shows the number of deaths in a seven-day rolling average in Florida in recent weeks.
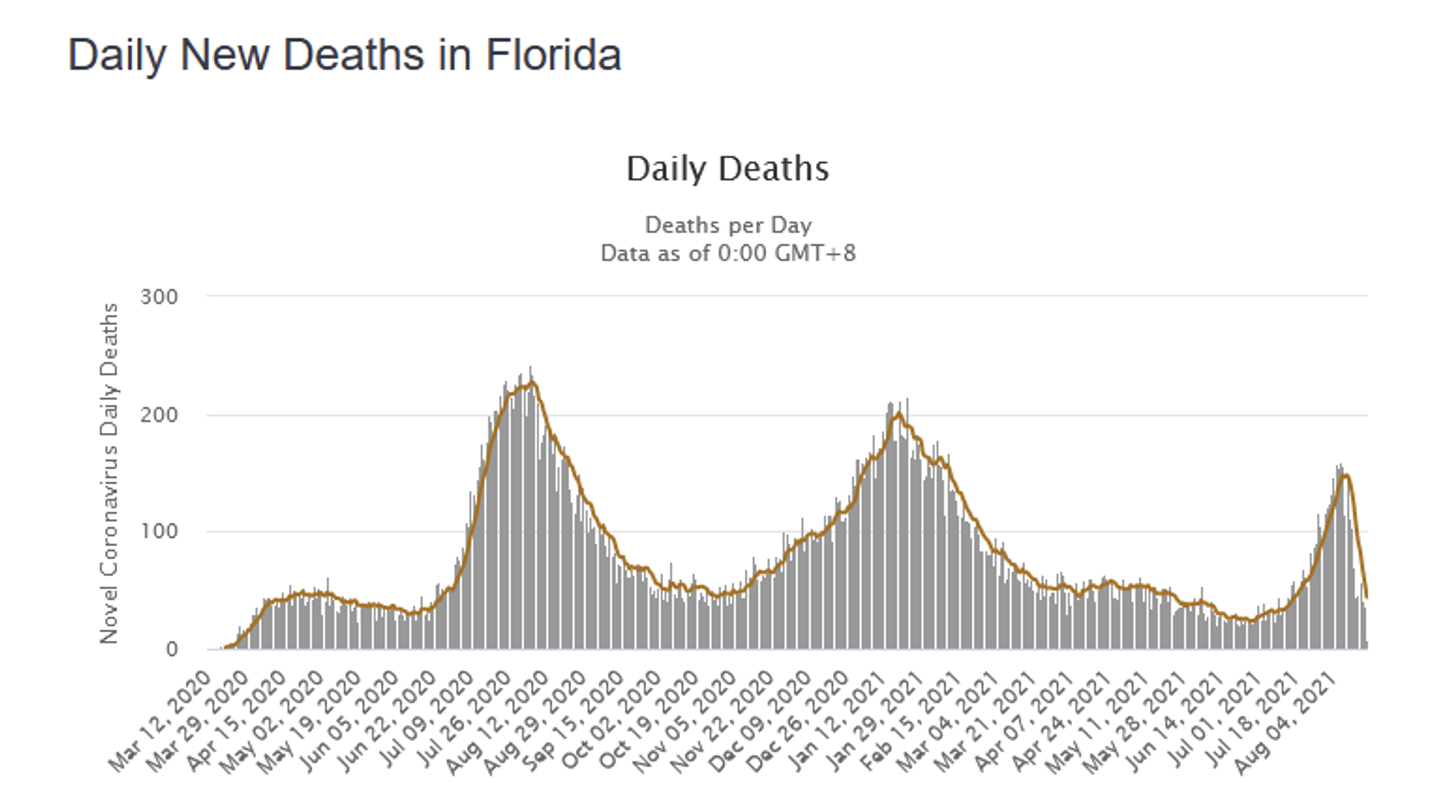
The number of deaths per day has declined to approximately 15 from a recent peak of 148 on August 8th. In Wisconsin, the picture is even better, with a seven-day rolling average of deaths at 3 that has not increased substantially even as case counts have risen.
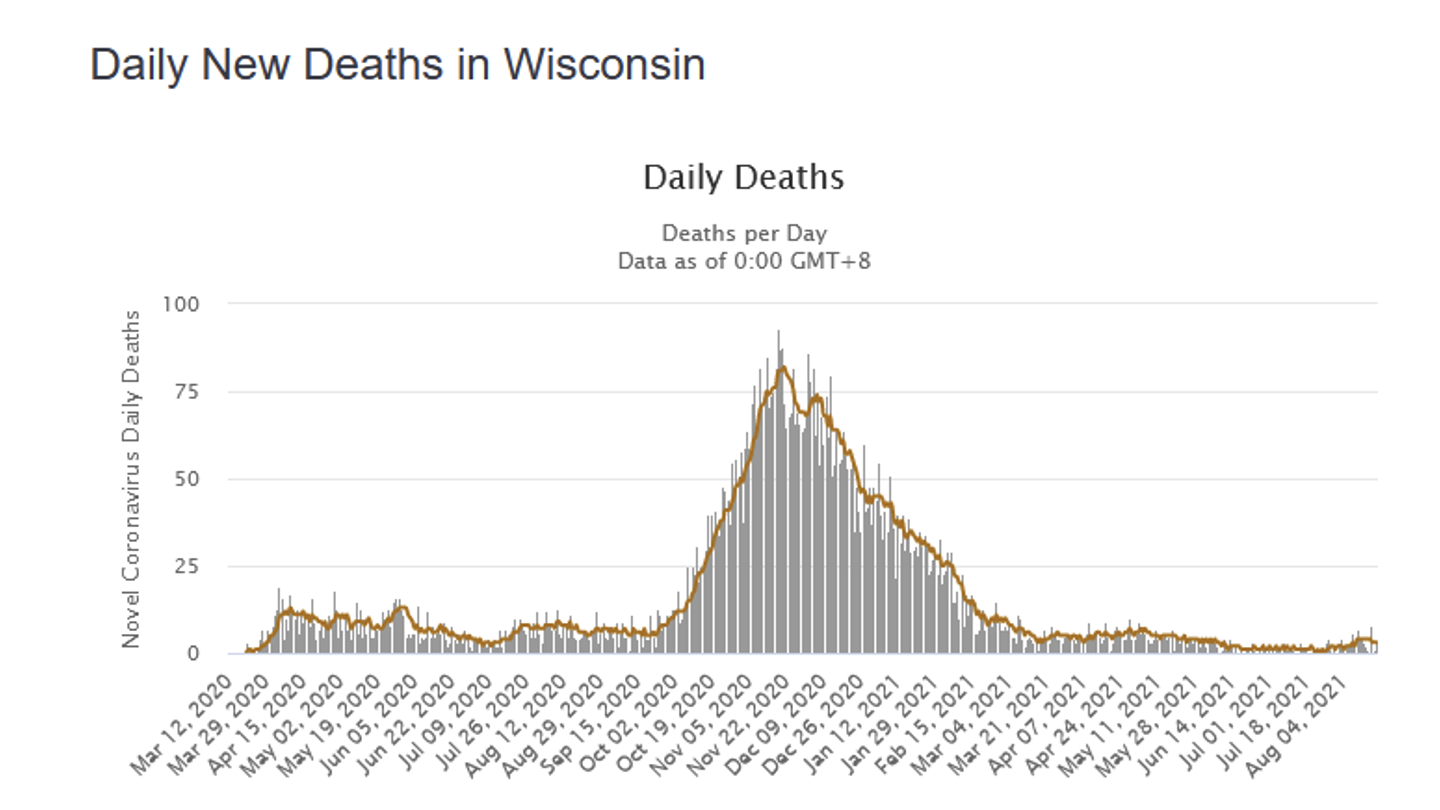
Why is this happening? A couple of reasons present themselves. First, the group most vulnerable to the coronavirus—the elderly—are the most highly vaccinated. Among those 65 and older in the state, about 84.4% have received a vaccine compared about 47.0% in the 18-24 age range. As cases move to younger and younger cohorts, the extent of hospitalizations and deaths inevitably declines with a virus that is affects the elderly the most. Second, given that the evolutionary incentive of a virus is to replicate, killing its host isn’t always optimal. Many viruses evolve to be less deadly over time, and we may be seeing that here.
Like the polarization of American politics across the board, there seems to be a need on the coronavirus to fall into one of two extreme camps. But finally bringing about a restoration of “normal” life will require us to ignore the loudest voices.